Case taking in Respiratory Diseases
by
Dr. Rajneesh Kumar Sharma MD (Homoeopathy) & Dr. (Km) Ruchi Rajput BHMS
Homoeo Cure Research Centre P. Ltd.
NH 74- Moradabad Road
Kashipur (UTTARANCHAL) - INDIA
Ph- 09897618594
Article outline- Structure of Case
History, Examination, Summary, Bibliography
In respiratory medicine the history taking will be done by both:
- Acute presentations – diagnosis must be quick but may be hindered by the patient’s condition
- Chronic presentations – documenting the key features in an illness that may span many years. Each situation has its specific challenges and in each a good history may reveal the diagnosis.
Initial observations
- Simple observation at the bedside can often give a good clue to the likely diagnosis:
- Inhalers and oxygen bottles
- Sputum pots
- Walking sticks or frames.
- How does the patient appear during the interview? Agitated, or distressed?
- Is there a visible tremor? Is the patient too breathless to speak in full sentences?
- Is the voice rough or hoarse?
- Simple observations now will save time later.
Structure of the Case history
Presenting complaint (PC)-
The presenting complaint is a concise statement of the symptoms felt by the patient. Patient’s own words should be used – this is not a diagnosis. Objectives
History of presenting complaint (HPC)-
A picture of the presenting complaint should be build up, investigating each symptom.
• Onset: acute or gradual
• Pattern: intermittent or continuous
• Frequency: daily, weekly or monthly
• Duration: minutes or hours
• Progression: better or worse than in the past
• Severity: mild, moderate or severe
• Character: e.g. is the pain sharp, dull or aching?
• Precipitating and relieving factors: e.g. are any medications used?
• Associated symptoms: e.g. cough, wheeze, haemoptysis, dyspnoea, chest pain, orthopnoea
• Systemic symptoms: e.g. fever, malaise, anorexia, weight loss.
Has the patient had the problem before? If so, what were the diagnosis, treatment and outcome? The patient should be asked how disabling the problem is and how it affects daily life. In patients with chronic illness, their exercise tolerance should be established whether this has declined.
Past medical history (PMH)-
PMH should be present the in chronological order, listing any hospital admissions, surgical operations and major illnesses.
Drug history (DH)
When taking the drug history, patient’s current intake of both prescribed and over-the-counter (OTC) drugs, recording dosage, frequency and duration of treatment should be listed.
Drug allergies
Patient should be asked about any allergies.
Family history (FH)
When noting a family history, it may be easier to draw a pedigree chart.
Social history (SH)
Social history is hugely important in the respiratory system; many respiratory diseases can be caused, or worsened, by social factors such as housing, occupation, hobbies or pets.
Smoking and alcohol
A detailed smoking history is essential. Record should be kept:
• Age started
• Age stopped (if applicable)
• Whether cigarettes, cigars or pipe
• Average smoked per day.
Occupation
Presentation of the patient’s jobs in chronological order starting from the time the patient left school is good. Hobbies may also be relevant.

Examination
General inspection
The initial observation is vital. Note should be made if any drip stands that are present, venous cannulae, or bandages.
Patient’s general appearance
Is the patient:
• Obviously unwell or distressed?
• Alert or confused?
• Thin or overweight?
There are some signs (e.g. use of accessory muscles of inspiration or pallor), cough (does it sound productive?). Is there any abnormality (e.g. hoarseness) in the voice?
Systematic general inspection
Muscle bulk, cachexia and skin in detail, thorax, how the patient is breathing, respiratory rate, signs of dyspnoea (e.g. use of accessory muscles of inspiration such as the sternomastoids etc. should be noticed.

Hands and limbs
Examination of the hands
The hands can reveal key signs of respiratory disease. Abnormally warm and cyanosed hands are a sign of CO2 retention. Fingers for nicotine staining, finger clubbing should be checked.


Examination of the pulse
A normal resting pulse in an adult is between 60–100 b.p.m. Bradycardia is defined as a pulse rate of less than 60 b.p.m. and tachycardia of greater than 100. Is the pulse regular and if not how is it irregular? In addition to testing pulse volume and character, which are better assessed from the carotid pulse, should also checked the presence of pulsus paradoxus. In normal individuals the pulse decreases slightly in volume on inspiration and systolic blood pressure falls by 3–5mmHg. In severe obstructive diseases (e.g. severe asthma) the contractile force of respiratory muscles is so great that there is a marked fall in systolic pressure on inspiration. A fall of greater than 10 mmHg is pathological.
Examination of the limbs
Axillary lymph nodes, ankles for oedema etc. should be checked. Bilateral pitting oedema is seen in many conditions including congestive cardiac failure, liver failure and cor pulmonale.
Head and neck
Examination of the face
• Signs of superior vena cava obstruction
• Cushingoid features
Mouth may give the signs of:
• Candida infection – white coating on tongue often seen after steroids or antibiotics
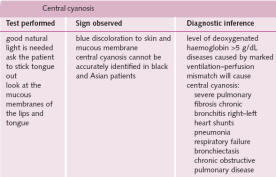
• Central cyanosis
Examination of the eyes and test for anaemia are also necessary.

Examination of the neck
Tracheal position and measurement of the cricosternal distance should be made Then patient at 45° should be tested for the jugular venous pulse. Finally, test for cervical lymphadenopathy from behind must be done.
Auscultation
Normal breath sounds are described as vesicular and have a rustling quality heard in inspiration and the first part of expiration. Examination must be done by-
• A logical order comparing the two sides
• With the patient taking fairly quick breaths through an open mouth.
Palpation
Patient should be palpated for any lumps or depressions and tested for the symmetry and extent of chest expansion. The apex beat should be in the fifth intercostal space at the midclavicular line. Test for tactile vocal fremitus should be done.
Percussion
The percussion note tells us the consistency of the matter underlying the chest wall, i.e. if it is air, fluid or solid. When percussing, it should be remembered that the upper lobe predominates anteriorly and the lower lobe predominates posteriorly. Palpation to determine tracheal position should be done. Sounds listen may be-
• Diminished vesicular breaths
• Bronchial breathing
• Added sounds, such as wheezes or stridor
• Crackles or
• Pleural rub
With auscultation BAR (B – Breath sounds; A – Added sounds; R – vocal Resonance) is important. Added sounds that disappear when the patient coughs are not significant.

Summary
Once examination is finished, sum up the positive findings in a clear and concise manner constitutes the complete pulmonary history. For Homoepathic purposes, a thorough case taking as per norms of Homoeopathy should be done and the above pulmonary case history must be merged into it to find out the similimum.
Bibliography
- An Introduction to the Symptoms and Signs of Surgical Diseases, Norman L. Browse
- Case Taking Work Book
- Current Medical Diagnosis & Treatment, Lawrence M. Tierney, Stephen J. McPhee
- Davidson’s Principles And Practice of Medicine
- Grant’s anatomy
- Gray’s anatomy
- Handbook of Human Physiology, Dr. Vidyaratan
- How to Take The Case & To Find the Similimum, E. B. Nash
- Human Physiology, Dr. Chandi Charan Chaterjee
- Pathology, Virginia A. LiVolsi, Maria J. Merino, John S. J. Brooks, Scott H. Saul, John E.
- Practice of Medicine, Dr. K. Chaudhury
- Principles of Internal Medicine Vol. I, II, Harrison
- Taber’s Cyclopedic Medical Dictionary
- Text Book Of Medical Physiology, Guyton